
HOW TO IDENTIFY NK
Neurotrophic keratitis (NK) shares many signs and symptoms with other common ocular conditions such as recalcitrant dry eye, so it may be underrecognized.1 Learn the importance of obtaining a patient’s full medical and treatment history in helping to detect NK before it progresses.
Patient case studies
PATIENT CASE STUDIES
EXPLORE the NK PATIENT JOURNEY TO DIAGNOSIS
Examine 3 potential neurotrophic keratitis (NK) patient cases to see how considering every aspect of a patient’s health can help you diagnose NK earlier on.
Select a patient to see how they were diagnosed with NK:

Diabetic retinopathy and a history of recalcitrant dry eye
43 years old
Living with type 2 diabetes and has a history of herpes simplex keratitis
62 years old

History of contact lens wear and ocular surgery
56 years old


History of contact lens wear and
ocular surgery
56 years old
Caucasian
Not an actual patient.
Ready to take a look at Linda’s NK diagnosis? It will only take a few minutes, and when we’re finished, you’ll be better prepared to recognize NK in your own practice and identify it before damage progresses.
Let’s get started!
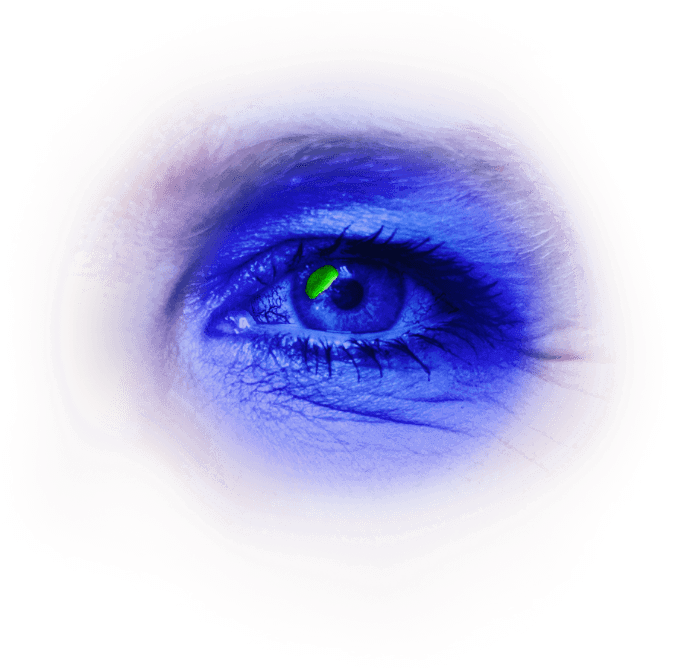
Linda, a patient with CHRONIC DRY EYE,
has undergone a comprehensive dry eye workup including slit lamp exams and vital dye staining. Today, she’s come to your practice complaining of photosensitivity so severe that she has trouble keeping her eye open.
Upon reviewing her chart, you see Linda’s best corrected visual acuity is 20/30.
Photosensitivity
Linda has been a patient in your practice for a long time, so you remember she has a 30-year history of
contact lens wear. As you continue to talk, you learn Linda also has a past medical history of hypertension and hyperlipidemia, which she manages with her primary care physician separately.
30 years of contact lens use
10 years of hypertension and hyperlipidemia
30 years of contact lens use
10 years of hypertension and hyperlipidemia
Upon initial slit lamp exam, you notice a possible epithelial defect on the superior nasal cornea of her left eye. In talking more with Linda, you recall she had LASIK surgery approximately 6 months ago and still wears contact lenses today.

LASIK surgery ~6 months ago
LASIK surgery ~6 months ago
Because Linda’s medical history—particularly her LASIK surgery and chronic contact lens use—may put her at higher risk for developing NK, you decide to find out more.1
Following Linda’s LASIK surgery, she was prescribed a topical antibiotic/steroid combination drop for 1 week and instructed to use artificial tears for a full month.

Prednisolone-moxifloxacin ophthalmic solution 3x daily for 1 week
Artificial tears 4x daily for 1 month
Prednisolone-moxifloxacin ophthalmic solution 3x daily for 1 week
Artificial tears 4x daily for 1 month
Artificial Tears
When Linda began experiencing dry eye symptoms, she started using artificial tears. Later, she was prescribed a steroidal ophthalmic solution for episodic use and additional anti-inflammatory dry eye drops.

Rx eye drops 2x daily
Artificial tears and steroid 4-6 weeks
Rx eye drops 2x daily
Artificial tears and steroid 4-6 weeks
Artificial Tears &
Steroids
When Linda’s dry eye persisted despite artificial tears and prescription eye drops, she transitioned to autologous serum eye drops, which she has been using for >3 months and is still using today.
At this point in your discussion with Linda, you have reason to believe Linda’s cornea may be damaged and decide to stain the eye.

Autologous serum eye drops >3 months
Autologous serum eye drops >3 months
In the event you need to test Linda’s corneal sensitivity, you decide not to use a vital dye containing anesthetic, and instead apply sterile saline to a vital dye staining strip.
Linda is so light sensitive that you have to hold her eye open to see the stained cornea. Examining her eye under cobalt blue light, you confirm an epithelial defect. Despite the amount of treatment Linda has been trying, it seems the cornea has only gotten worse over time.
Considering this persistent epithelial defect in combination with everything you now know about Linda’s medical and treatment history, you suspect her corneal sensitivity may be reduced as a result of NK. The only way to confirm your diagnosis is with corneal sensitivity testing, which you decide to do next.
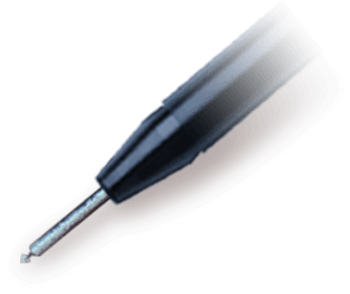
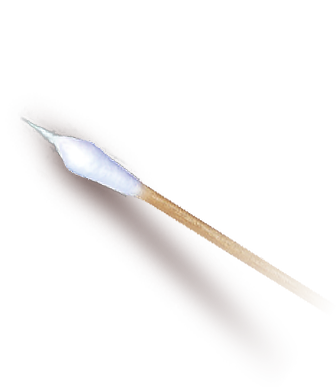
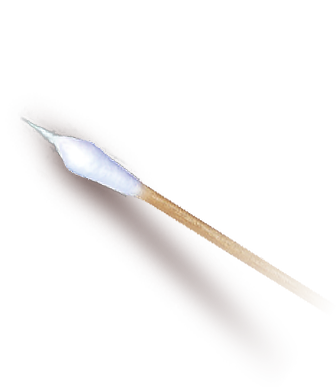
Using a cotton-tipped applicator shaped into a thin wisp, you first test Linda’s healthy eye to establish a baseline. Then, you test the damaged quadrant of Linda's cornea, followed by the center and remaining quadrants. She has no reaction whatsoever, suggesting corneal sensitivity is absent.

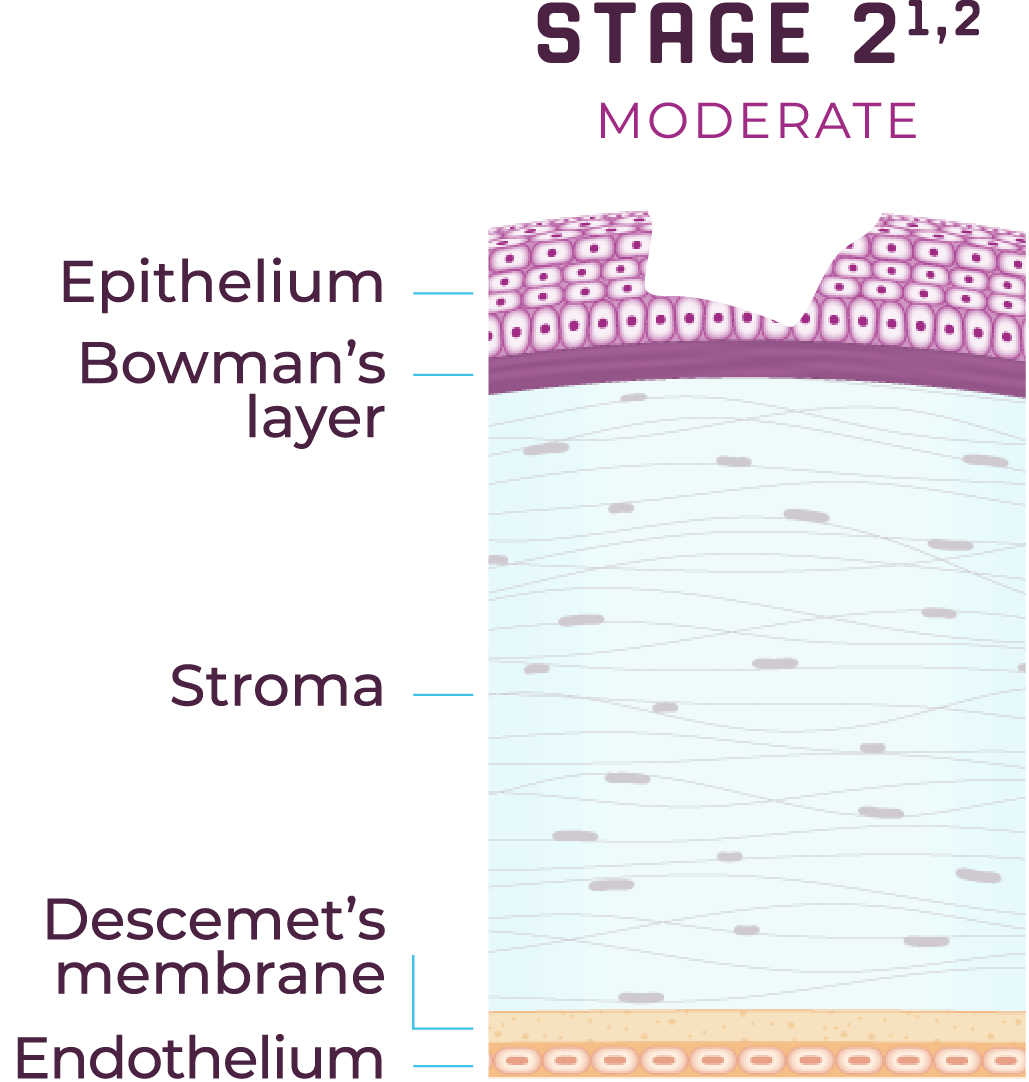
Based on Linda’s medical history, absent corneal sensitivity, and the persistent epithelial defect confirmed upon staining, you diagnose Linda with Stage 2 NK.1,2
As you can see, without asking about Linda’s medical history, her NK could have been continuously misdiagnosed.1 By noticing common signs and symptoms of NK and recognizing potential causes, you can work to manage Linda appropriately.
Not an actual patient.
Not an actual patient.
Great work! Now experience another patient’s journey to NK diagnosis.
Living with type 2 diabetes and has a history of herpes simplex keratitis
62 years old
Not an actual patient.

Diabetic retinopathy and a history of recalcitrant dry eye
43 years old
Not an actual patient.
References: 1. Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res. 2018;66:107-131. 2. Mastropasqua L, Massaro-Giordano G, Nubile M, Sacchetti M. Understanding the pathogenesis of neurotrophic keratitis: the role of corneal nerves. J Cell Physiol. 2017;232(4):717-724.



Living with type 2 diabetes and has a
history of herpes simplex keratitis
62 years old
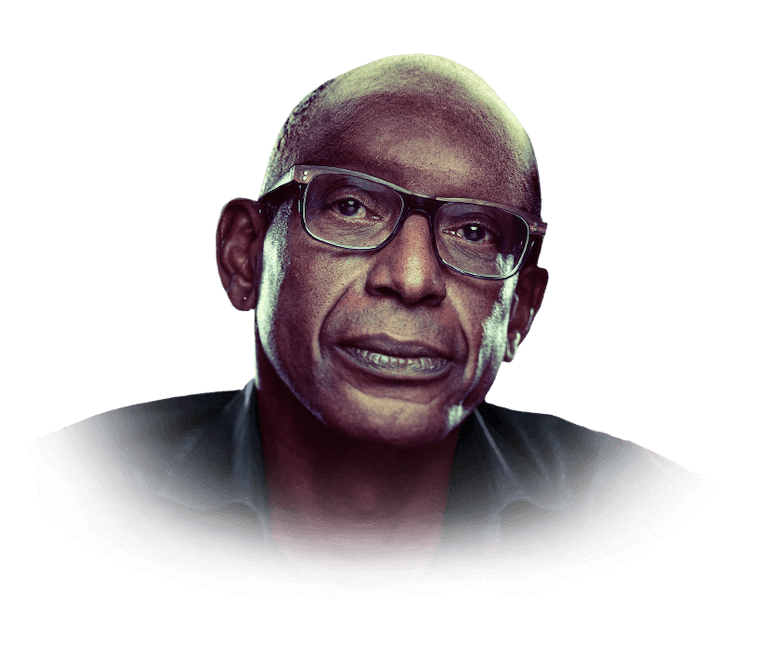
African American
Not an actual patient.
Let’s take a few minutes to understand Carl’s NK diagnosis. When we’re finished, you’ll be better prepared to suspect NK in your own practice and identify this rare disease that often goes unrecognized before it progresses.1
Let’s get started!
Carl is a new patient and has come to his appointment with you today complaining of fluctuating vision and a tired feeling in his eyes. Upon initial examination, you confirm visual acuity is reduced in his right eye. You also notice trace corneal neovascularization in his right eye during a slit lamp exam.

VA OD 20/50
VA OS 20/25
As you continue Carl’s initial exam, you learn he’s been struggling with

Long history of dry eye
Long history of dry eye
You spend some more time with Carl to learn about his medical history. He seems to be in good health but lets you know he has Type 2 diabetes. When you ask about his A1C, Carl admits he’s struggled to keep it below 8% for years. As you continue the discussion, Carl also shares he has a history of HERPES SIMPLEX KERATITIS (HSK) and experienced an episode about 2 years ago.

HSK episode ~2 years ago
HSK episode ~2 years ago
Type 2 DM
A1C >8.0%
You know that Carl’s comorbidities put him at higher risk for developing NK, so you decide to ask about his treatment history.2
To manage his HSK, Carl has a prescription for oral antivirals, which he has been taking for several years. To deal with chronic dry eye, Carl began using artificial tears early in his treatment and relied on them for years.


Oral antiviral
Years of artificial tear use
Oral antiviral
Years of artificial tear use
Oral
Antiviral Rx
In the past, when Carl continued to experience dry eye symptoms, his previous eye doctor prescribed anti-inflammatory eye drops and inserted a punctal plug in the lower lid.


Anti-inflammatory eye drops
1 punctal plug insertion in lower lid punctum
Anti-inflammatory eye drops
1 punctal plug insertion in lower lid punctum
Anti-inflammatory
Eye Drops
Unfortunately, the anti-inflammatory eye drops and punctal plug did not adequately control the symptoms of dry eye in Carl's right eye. As Carl’s dry eye worsened, his previous eye doctor placed a self-retaining amniotic membrane on 2 separate occasions.
At this point in your discussion with Carl, you have reason to believe his cornea may be damaged and decide to stain the eye.


2 separate placements of a self-retaining
amniotic membrane
2 separate placements of a self-retaining amniotic membrane
You decide not to numb the eye before staining in case you need to test Carl’s corneal sensitivity. Instead, you use vital dye stain strips to stain Carl’s eye.


Examining the stained eye under cobalt blue light, you discover nasal confluent SPK.
As you consider the findings of your staining along with everything you learned about Carl’s medical history, treatment history, and worsening dry eye, you suspect his corneal sensitivity may be compromised and decide to perform corneal sensitivity testing.

Using a cotton-tipped applicator formed into a thin wisp, you test the center and each quadrant of Carl’s cornea, after first testing his healthy eye as a baseline. As you suspected, his corneal sensitivity is reduced.

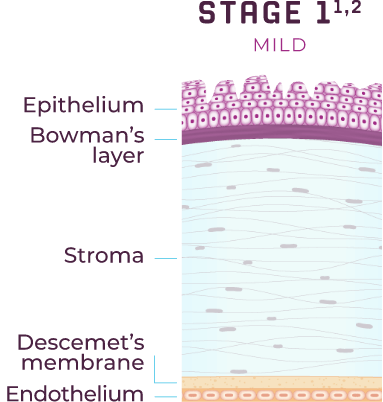
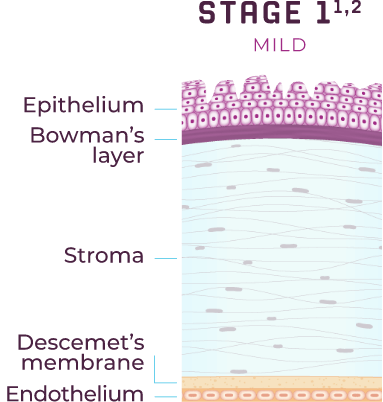
Considering Carl’s reduced corneal sensitivity and the punctate keratitis revealed upon staining, you diagnose Carl with Stage 1 NK.1,2

As you can see, without considering Carl's medical history and testing corneal sensitivity, his NK could have gone unrecognized. It’s important to consider NK if you see persistent corneal epithelial staining that does not heal.

Not an actual patient.
Not an actual patient.
Great work! Now experience another patient’s journey to NK diagnosis.

Diabetic retinopathy and a history of recalcitrant dry eye
43 years old
Not an actual patient.

History of contact lens wear
and ocular surgery
56 years old
Not an actual patient.
References: 1. Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res. 2018;66:107-131. 2. Mastropasqua L, Massaro-Giordano G, Nubile M, Sacchetti M. Understanding the pathogenesis of neurotrophic keratitis: the role of corneal nerves. J Cell Physiol. 2017;232(4):717-724.




Diabetic retinopathy and a history of
recalcitrant dry eye
43 years old
Latina
Not an actual patient.
Now let’s review Sofia’s NK diagnosis to help you be better prepared to suspect NK in your own practice and identify this rare disease that often goes unrecognized before it progresses.1
Let’s get started!
Sofia is a long-time patient in your practice. You diagnosed her with RECALCITRANT DRY EYE in the past, but despite previous treatments, she is still experiencing symptoms and has come to her appointment today looking to address this. Upon initial examination, you see Sofia’s right corneal epithelium is dry and cloudy.

Cloudy corneal epithelium
Cloudy corneal epithelium
Symptoms of Dry Eye
Upon reviewing Sofia's chart, you're reminded she hasTYPE 2 DIABETES and struggles to keep her A1C under control.
You also recall Sofia has been diagnosed with bilateral DIABETIC RETINOPATHY, a result of her poorly controlled blood sugar.

Bilateral diabetic retinopathy
Bilateral diabetic retinopathy
Type 2 DM
A1C >8.0%
Sofia’s chart also includes her history of contact lens wear. Sofia has been wearing contact lenses since before she came to your practice, and you see that her best corrected distance visual acuity is 20/40.

Contact lens wear for 20 years
BCDVA 20/40
Contact lens wear for 20 years BCDVA 20/40
Because Sofia’s poorly controlled diabetes and long-term contact lens wear put her at risk for developing NK, you decide to revisit her treatment history.1,2
For her recalcitrant dry eye disease, Sofia began using artificial tears in both eyes and continued to use them for years. Later, you prescribed Sofia autologous serum eye drops, which she used bilaterally for approximately 6 months.


Autologous serum eye drops
>6 months
Autologous serum eye drops >6 months
Artificial Tears
When the artificial tears and autologous serum did not sufficiently manage Sofia’s dry eye symptoms, you decided to prescribe her anti-inflammatory eye drops along with an ophthalmic corticosteroid. Despite these treatments, Sofia’s redness and visual fluctuation with lenses have not improved.


Ophthalmic corticosteroid
Ophthalmic corticosteroid
Anti-inflammatory
Eye Drops
Sofia also has a retina specialist who has been managing her diabetic retinopathy (DR).
The specialist decided to start Sofia on intravitreal anti-VEGF (vascular endothelial growth factor) treatment. Following the initial dose of 1 injection every 4 weeks for 5 months, Sofia now receives 1 injection in her right eye every 8 weeks to control her DR and help improve her vision.


IVT anti-VEGF once every 8 weeks
IVT anti-VEGF once every 8 weeks
The cloudy corneal epithelium in Sofia's right eye and recalcitrant dry eye disease lead you to believe her cornea may be damaged, so you decide to stain her right eye using vital dye containing anesthetic.


While examining Sofia’s stained eye under cobalt blue light, you identify inferior temporal SPK.
Considering the corneal damage in conjunction with Sofia’s comorbidities and treatment history, you suspect corneal sensitivity in her right eye may be reduced as a result of NK. But as her eye is currently numb from the anesthetic, you ask Sofia to return in a week to perform corneal sensitivity testing.

At Sofia's next visit, before any drops are instilled, you use a cotton-tipped applicator pulled into a thin wisp to test the sensitivity of Sofia’s healthy eye as a baseline. Then, you test her damaged eye, starting with the quadrant of the cornea where the SPK is located before testing the remaining quadrants and center.
As you suspected, sensitivity in Sofia's right eye is reduced.

Taking into consideration Sofia's medical history, reduced corneal sensitivity, and moderate SPK, you diagnose her with Stage 1 NK.1,2
As you can see, without reexamining Sofia's medical history and previous diagnoses, her NK could have continued to be missed. It's important to consider NK in diabetic patients with symptoms of recalcitrant dry eye.

Not an actual patient.
Not an actual patient.
Great work! Now experience another patient’s journey to NK diagnosis.
Living with type 2 diabetes and has a history of herpes simplex keratitis
62 years old
Not an actual patient.

History of contact lens wear
and ocular surgery
56 years old
Not an actual patient.
References: 1. Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res. 2018;66:107-131. 2. Mastropasqua L, Massaro-Giordano G, Nubile M, Sacchetti M. Understanding the pathogenesis of neurotrophic keratitis: the role of corneal nerves. J Cell Physiol. 2017;232(4):717-724.
References: 1. Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res. 2018;66:107-131. 2. Mastropasqua L, Massaro-Giordano G, Nubile M, Sacchetti M. Understanding the pathogenesis of neurotrophic keratitis: the role of corneal nerves. J Cell Physiol. 2017;232(4):717-724.
Sign up for updates
Sign up for updates
COMMON CAUSES
Common Causes
ETIOLOGIES AND RISK FACTORS OF NK
Loss of corneal sensitivity can result from a number of etiologies and can lead to neurotrophic keratitis (NK).1 A thorough evaluation of a patient’s medical history is the first step to help you identify potential risk factors for NK.2 In particular, it is important to know if your patient has had herpetic eye disease or is living with poorly controlled diabetes, as both can lead to loss of corneal sensitivity.2
Ocular1
- Post-herpetic infection
- Ocular surgery (LASIK, cataract surgery, corneal transplantation, vitrectomy)
- Contact lens wear
- Topical ophthalmic drug toxicity
- Chemical and physical burns
Systemic1
- Diabetes
- Multiple sclerosis
- Vitamin A deficiency
- Leprosy
- Amyloidosis
Central Nervous System1
- Post-neurosurgical procedures
- Stroke
- Neoplasm
- Aneurysms
- Degenerative CNS disorders
Genetic1
- Riley-Day syndrome
- Goldenhar-Gorlin syndrome
- Moebius syndrome
- Familial corneal hypoesthesia
SIGNS & SYMPTOMS
Signs & Symptoms
PRESENTATION OF NK
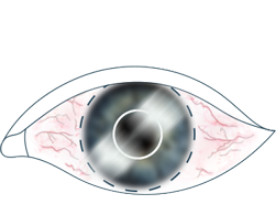
Though many etiologies can contribute to the development of neurotrophic keratitis (NK), it is considered to be its own clinical entity, and not a complication of disease(s).2
Signs and symptoms of NK depend on the severity of the disease. Early on, patients may complain of dryness, photophobia, or trouble reading for prolonged periods due to reduced tear production and reduced blinking. Visual impairment may be present but may worsen with disease severity and lesion location.1
Keep in mind that because decreased corneal sensitivity is the hallmark of NK, some patients may not complain of symptoms.1 These patients typically wait to seek medical advice until after the disease has progressed.1

Dryness
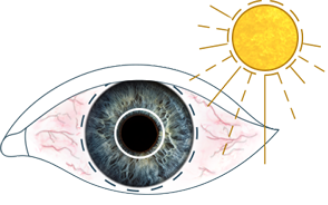
Photophobia
blurred vision

Reduced Blinking
IDENTIFY NK THROUGH CORNEAL SENSITIVITY TESTING
Neurotrophic keratitis (NK) can develop as a result of a number of causes and be mistaken for other common ocular conditions.1 Testing corneal sensitivity is essential to an accurate and timely diagnosis.1
Sign up to stay in the know about nk
References: 1. Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res. 2018;66:107-131. 2. Mastropasqua L, Massaro-Giordano G, Nubile M, Sacchetti M. Understanding the pathogenesis of neurotrophic keratitis: the role of corneal nerves. J Cell Physiol. 2017;232(4):717-724.