
CORNEAL SENSITIVITY TESTING IS KEY TO NK DIAGNOSIS
Because decreased corneal sensitivity is the hallmark sign of neurotrophic keratitis (NK), corneal sensitivity testing should be performed as soon as it is suspected.1 Learn about different testing methods, ways to include them in your diagnostic workflow, and recommendations for reaching an accurate diagnosis.
Diagnostic Approach
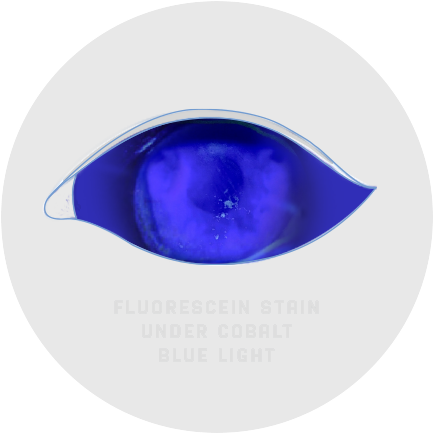
CONSIDERATIONS FOR STAIN WITHOUT PAIN
Slit lamp examination and vital dye staining can reveal signs such as1-4:
- Cloudy or irregular corneal epithelium; punctate epithelial keratitis (PEK), also referred to as superficial punctate keratitis (SPK) or punctate epithelial erosions (PEE)
- Persistent epithelial defects (PED)
- Corneal ulcers
If these signs don’t respond to therapy, it may be an indicator of neurotrophic keratitis (NK) and warrant further diagnostic evaluation to assess for decreased corneal sensitivity.1
IT’S IMPORTANT NOT TO NUMB THE EYE WHEN PERFORMING STAINING.
If numbing drops must be used, make a note in the patient’s record to perform corneal sensitivity testing during their next visit before using topical drops.
An alternative to using vital dyes combined with anesthetic drops is using vital dye staining strips, which apply a controlled amount of dye, allowing for better visualization of the corneal surface.5 If the patient does not react to the strip touching the eye, it may be indicative of impaired corneal sensitivity and a sign of NK.1
If NK is suspected, corneal sensitivity testing should be conducted to confirm a diagnosis.
Testing Methods
QUALITATIVE AND QUANTITATIVE TESTS
Because neurotrophic keratitis (NK) often presents similarly to more common ocular conditions, such as dry eye, corneal sensitivity testing is the key for making a diagnosis.1
There are 2 common ways to test—one qualitative, the other quantitative—but many practices find qualitative methods to be most practical and efficient1:
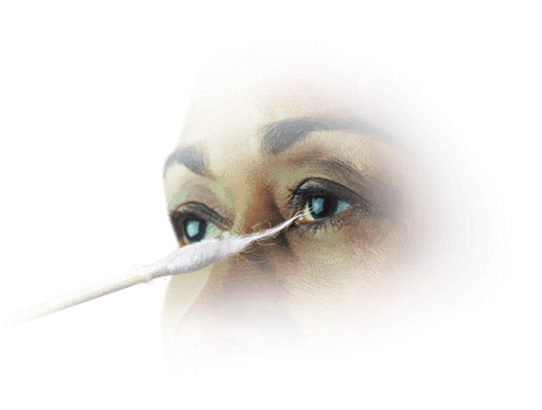
COTTON-TIPPED APPLICATOR1
The cotton-tipped applicator or dental floss are easily accessible, sterile, and disposable qualitative tests for NK. They allow for a comparison of sensation in each eye. Consider testing the healthy eye first to establish a baseline before testing the damaged eye.
To conduct corneal sensitivity testing, approach the patient from the side and test the center and all 4 quadrants of the eye. When the cotton thread gently touches the cornea, normal subjects show a blink reaction and can describe the sensation of touch, while patients with loss of corneal sensitivity do not react. Record sensations as “normal,” “reduced,” or “absent.”

Cochet-Bonnet esthesiometer1
To quantitatively test corneal sensitivity, consider the Cochet-Bonnet esthesiometer. The device contains a thin nylon microfilament that retracts incrementally, measuring sensitivity by the length of the filament required to produce a blink reaction. To conduct the test, extend the filament to full length (60 mm) and retract 5 mm at a time until the patient feels contact. Record the length and compare to the healthy eye.
Testing Instructions
When testing corneal sensitivity, remember s.i.g.n.
Set a baseline by testing the healthy eye first.1
Investigate the suspected eye starting with the damaged area or the center of the cornea.
Gently touch the testing tool to the cornea.1
Note the patient’s reaction and record sensation.1

For the most precise examination, test all 4 quadrants of the cornea as well as the center and compare sensation to the healthy eye.1
As the center of the eye is the most sensitive area of the ocular surface, some eye care professionals prefer to test only the center of the cornea to determine if a patient has neurotrophic keratitis (NK). Others test only the area of the cornea with visible damage.6
References: 1. Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res. 2018;66:107-131. 2. Mastropasqua L, Massaro-Giordano G, Nubile M, Sacchetti M. Understanding the pathogenesis of neurotrophic keratitis: the role of corneal nerves. J Cell Physiol. 2017;232(4):717-724. 3. Versura P, Giannaccare G, Pellegrini M, Sebastiani S, Campos EC. Neurotrophic keratitis: current challenges and future prospects. Eye Brain. 2018;10:37-45. 4. Roussel T, Grutzmacher R, Coster D. Patterns of superficial keratopathy. Aust J Ophthalmol. 1984;12(4):301-316. 5. Starr CE, Gupta PK, Farid M, et al. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refract Surg. 2019;45(5):669-684. 6. Mirzajan A, Khezri F, Jafarzadehpur E, Karimian F, Khabazkhoob M. Normal corneal sensitivity and its changes with age in Tehran, Iran. Clin Exp Optom. 2015;98(1):54-57.