Test for NK as it may progress
CORNEAL SENSITIVITY TESTING IS KEY TO NK DIAGNOSIS
Because decreased corneal sensitivity is a key characteristic of neurotrophic keratitis (NK), corneal sensitivity testing should be performed as soon as it is suspected.1 Learn about different testing methods, ways to include them in your diagnostic workflow, and recommendations for reaching an accurate diagnosis.
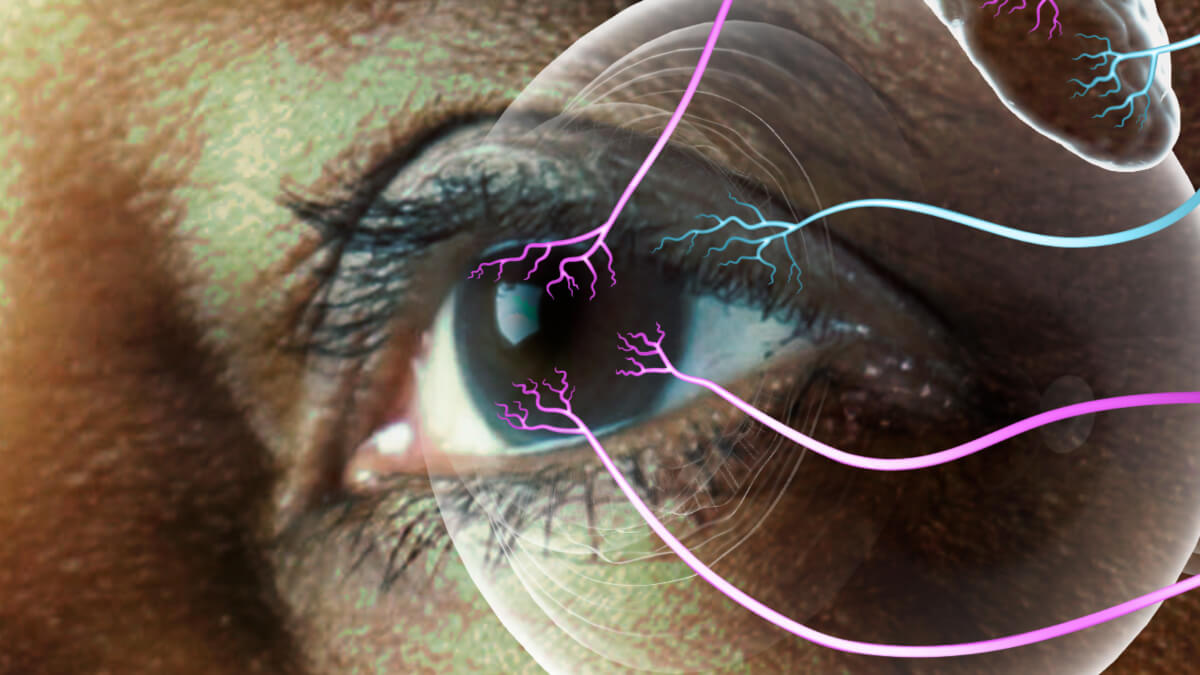
The image is for illustrative purposes only.
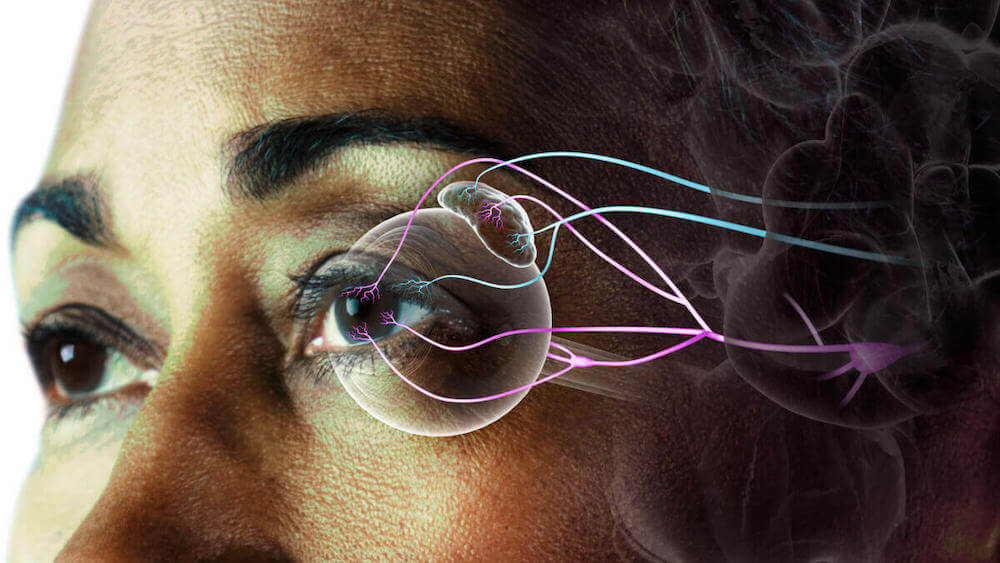
The image is for illustrative purposes only.
IMPORTANCE OF CORNEAL SENSITIVITY
CORNEAL NERVES HELP MAINTAIN OCULAR SURFACE HOMEOSTASIS
By providing nourishment to the ocular surface and stimulating protective reflexes, such as blinking and tear production, healthy corneal nerves help maintain corneal integrity and homeostasis.2 Corneal sensitivity is a key indicator of corneal nerve function.2
Ocular surface homeostasis is maintained by an intricate feedback loop of corneal nerves, the lacrimal gland, and the corneal epithelium represented by moving arrows in the illustration below.1,2
Select each number to learn about the steps involved in maintaining ocular surface homeostasis.
Corneal nerves, represented by arrows moving away from the eye, send sensory information to the brain.1
Corneal nerves trigger protective reflexes, represented by arrows moving toward the eye, such as tear production and blinking.2
Corneal nerve fibers release neuromediators that promote nourishment to the cornea and stimulate healing.2
Nerve growth factor (NGF), NT-3, BDNF, and NT-4 are neurotophins present in the corneal epithelium that aid in maintaining ocular surface homeostasis by supporting the survival and maturation of corneal nerve fibers (as shown in preclinical models).2-4
Diagnostic Approach
CONSIDERATIONS FOR RECOGNIZING NK
Slit lamp examination and vital dye staining can reveal signs such as1,2,5,6:
- Cloudy or irregular corneal epithelium; superficial punctate keratitis (SPK)
- Persistent epithelial defects (PED)
- Corneal ulcers
If these signs don’t respond to therapy, it may be an indicator of neurotrophic keratitis (NK) and warrant further diagnostic evaluation to assess for decreased corneal sensitivity.1
IF NK IS SUSPECTED IT IS IMPORTANT NOT TO NUMB THE EYE DURING STAINING AS THIS WILL IMPACT YOUR ABILITY TO CONDUCT CORNEAL SENSITIVITY TESTING.5
If numbing drops must be used, make a note in the patient’s record to perform corneal sensitivity testing during their next visit before using topical drops.
An alternative to using vital dyes combined with anesthetic drops is using vital dye staining strips, which apply a controlled amount of dye, allowing for better visualization of the corneal surface.7 If the patient does not react to the strip touching the eye, it may be indicative of impaired corneal sensitivity and a sign of NK.1
If NK is suspected, corneal sensitivity testing should be conducted to confirm a diagnosis.
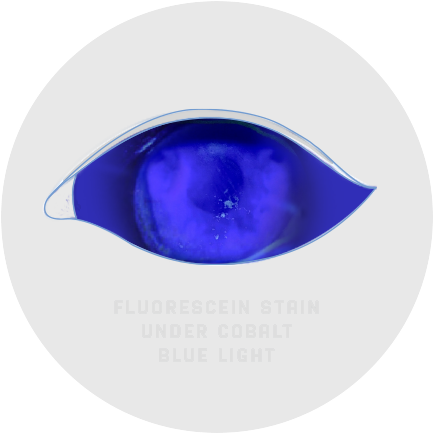
The image is for illustrative purposes only. This is not an exact representation of a patient, or a structure and function.
Corneal Sensitivity Testing Methods
QUALITATIVE AND QUANTITATIVE TESTS
Because neurotrophic keratitis (NK) often presents similarly to more common ocular conditions, such as dry eye, corneal sensitivity testing is important for making a diagnosis.1,8
Methods of corneal sensitivity testing include the cotton wisp (qualitative) and the Cochet-Bonnet esthesiometer (quantitative).1
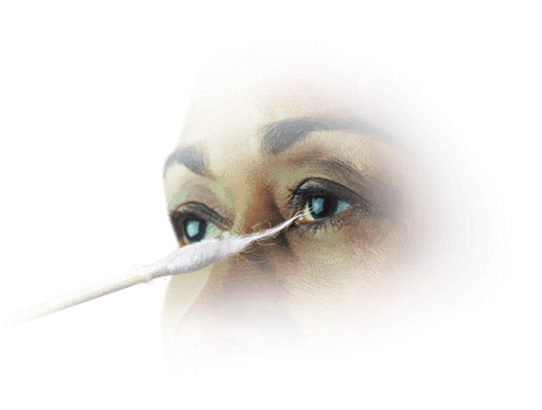
COTTON-TIPPED APPLICATOR1,9
The cotton-tipped applicator is an easily accessible and disposable qualitative test for NK. They allow for a comparison of sensation in each eye. Consider testing the healthy eye first to establish a baseline before testing the damaged eye.
To conduct corneal sensitivity testing, approach the patient from the side and test the center and all 4 quadrants of the eye. When the cotton thread gently touches the cornea, normal subjects show a blink reaction and can describe the sensation of touch, while patients with loss of corneal sensitivity do not react. Record sensations as “normal,” “reduced,” or “absent.”

Cochet-Bonnet esthesiometer1
One way to quantitatively test corneal sensitivity, consider the Cochet-Bonnet esthesiometer. The device contains a thin nylon microfilament that retracts incrementally, measuring sensitivity by the length of the filament required to produce a blink reaction. To conduct the test, extend the filament to full length (60 mm) and retract 5 mm at a time until the patient feels contact. Record the length and compare to the healthy eye.
The images are for illustrative purposes only. These are not an exact representation of a patient, or a structure and function.
Identifying NK
PERFORMING A CORNEAL SENSITIVITY TEST
Watch a step-by-step tutorial on corneal sensitivity testing conducted by corneal specialist Francis Mah, MD.
A full transcript of the video is available here.
References: 1. Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res. 2018;66:107-131. 2. Mastropasqua L, Massaro-Giordano G, Nubile M, Sacchetti M. Understanding the pathogenesis of neurotrophic keratitis: the role of corneal nerves. J Cell Physiol. 2017;232(4):717-724. 3. Qi H, Chuang EY, Yoon KC, et al. Patterned expression of neurotrophic factors and receptors in human limbal and corneal regions. Mol Vis. 2007;13:1934-1941. 4. Di G, Qi X, Zhao X, et al. Corneal epithelium-derived neurotrophic factors promote nerve regeneration. Invest Ophthalmol Vis Sci. 2017;58(11):4695-4702. 5. NaPier E, Camacho M, McDevitt T, Sweeney AR. Neurotrophic keratopathy: current challenges and future prospects. Ann Med. 2022;54(1):666-673. 6. Versura P, Giannaccare G, Pellegrini M, Sebastiani S, Campos EC. Neurotrophic keratitis: current challenges and future prospects. Eye Brain. 2018;10:37-45. 7. Starr CE, Gupta PK, Farid M, et al. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refract Surg. 2019;45(5):669-684. 8. Dana R, Bradley JL, Guerin A, et al. Estimated prevalence and incidence of dry eye disease based on coding analysis of a large, all-age United States health care system. Am J Ophthalmol. 2019;202:47-54. 9. Sacchetti M, Lambiase A. Diagnosis and management of neurotrophic keratitis. Clin Ophthalmol. 2014;8:571-579.